2017 Birthing Justice Forum: “No Mas Bebes”& Maternal-Child Health Champion Awards Ceremony
Wednesday, September 27, 2017
8:30 am to 6:00 pm
California Endowment Center, Los Angeles, CA
Download PDF: Historical Timeline for Reproductive and Birthing Justice & Natural Childbirth Movement
Promoting Human Rights in Maternity Care for all Childbearing Persons
“The Struggle Shall Not Deter Us from A Cause We Believe to Be Just”
 Attendees, Speakers and Volunteers at The 2017 Birthing Justice Forum (Photography Courtesy Ani Tsatourian, http://aniportraits.com).
Attendees, Speakers and Volunteers at The 2017 Birthing Justice Forum (Photography Courtesy Ani Tsatourian, http://aniportraits.com).
Audience: Perinatal & Public Health Nurses, Physicians, Midwives, Doulas, Social Workers, Marriage & Family Therapists, Childbirth Educators, Lawyers, Community Health Promoters, Certified Health Education Specialists, Family Health Advocates, Perinatal Home Visitors & Case Managers, Certified Perinatal Health Workers, Reproductive Health Workers, Parents and Grandparents
Featuring the Documentary film by Renee Tajima-Pena and Virginia Espino
NO MAS BEBES/NO MORE BABIES
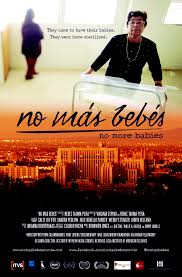
They came to have their babies. They went home sterilized. The story of Mexican immigrant women who were sterilized at LA county hospital during the 1970s. Alongside young Chicana/o lawyers and a whistle-blowing doctor, they stood up to powerful institutions in the name of justice.
Vinieron a tener sus bebes. Se fueron a casa esterilizados. La historia de las mujeres inmigrantes mexicanas que fueron esterilizadas en el hospital del Condado de la cada de 1970. Junto a los juvenes abogados de chicana y un medico que soplaba silbato, se enfrentaban a instituciones poderosas en nombre de la justicia.
Eugenics (u-GEN-icks) (noun): “The study of methods of improving the quality of the human race, especially by selective breeding.”
Film Synopsis:
“They came to have their babies. They went home sterilized. The story of immigrant mothers who sued county doctors, the state, and the U.S. government after they were pushed into sterilizations while giving birth at the Los Angeles County-USC Medical Center during the 1960s and 70s. Led by an intrepid, 26-year-old Chicana lawyer and armed with hospital records secretly gathered by a whistle-blowing young doctor, the mothers faced public exposure and stood up to powerful institutions in the name of justice” (No Mas Bebes, n.d.).
In another yet another example of institutionalized racism, the court sided with LAC+USC and Dr. Quilligan, but the case set the precedent for Informed Consent Forms to be provided to persons receiving health care in their native language.
This sad chapter in American and specifically Los Angeles history, shows what communities of color, attorneys, advocates for mothers and children, and medical professionals can do when they are empowered and build alliances to stand up to injustice and bring about change.
We asked the following questions at this event:
- What injustices in maternity care do we know are going on today?
- What can we do about it?
- What would reparations for persons harmed by Birthing Injustices look like?
We care about women and children, birthing rights, human rights, social inequities, health disparities, racism and oppression, so we are engaged in this conversation and plan for action and community empowerment. Together, we are joining forces to bring about real solutions and improve health care for all childbearing persons.
WHO ATTENDED THIS CONFERENCE?
Midwives, doulas, educators, policymakers, mental health professionals, reproductive rights activists, nurses, students, mothers and grandmothers.
DESCRIPTION OF CONFERENCE

2017 Maternal-Child Health Champion Awardees: “Si, Se Puede!”
We came together in this forum to discuss issues of perinatal heath inequities from a human rights perspective. Using the film NO MAS BEBES/NO MORE BABIES as a springboard for our discussion and action, attendees heard from a panel of maternal-infant health researchers, activists, advocates, midwives, doulas, physicians, psychologists and reproductive and birthing rights experts about the socio-political influences on poor birth outcomes in communities of color. Caucasian maternal-health professionals leaned what they can do to support the efforts of birth activists and birth professionals of color and how to effectively work with and advocate for their clients of color.
Maternity care providers and childbirth activists, maternal-infant advocates alike are working to make birth safer and more satisfying for pregnant people everywhere. While all agree that all pregnant people ought to have access to quality care during pregnancy, not everyone receives equal treatment or equal caliber of care in America and elsewhere.
Following the panel and film, we participated in a group interactive exercise based on the Socioecological Model to work on strategies to impact change in maternity care and birth outcomes.
The Maternal-Child Health Champion Awards Ceremony followed the forum, to recognize leaders in the community.
LEARNER OBJECTIVES
1.Discuss how historical injustices occurring among women of color in the U.S. impact physical and mental health of mothers and children.
2.Describe four human rights of childbearing persons.
3.Apply the socio-ecological framework to address domains of influence on perinatal health inequities and disparities.
4. Develop an action plan/community intervention to create positive social change to transform social/individual determinants of perinatal health
PANEL DISCUSSION
Following the film, there was a panel discussion about birthing justice with birthing and reproductive rights activists and the filmmaker, Virginia Espino, Ph.D.

PANELISTS
- Virginia Espino, Filmmaker
- Ena Valladares, MPH, California Latinas for Reproductive Justice
- Dr. Sayida Peprah, Psy.D
- Chemin Perez, LM, CPM, Arcadia Birth Center/Nueva Vida Parteria
MATERNAL-CHILD HEALTH CHAMPION AWARDS CEREMONY
Maternal-Child Health Champion Awards Ceremony followed the symposium. Exemplary MCH practitioners an activists were recognized for their ingenuity, audacity, boldness, and potential in making a profound difference in the lives of mothers and infants, and improving maternity care quality.
2017 AWARDEES
Agent-Provocateur of the Year: Monica McLemore, RN, MPH, Ph.D., Researcher & Educator and Associate Professor, UCSF School of Nursing
Description: To honor a person who has demonstrated revolutionary ingenuity in developing programs and projects promoting the health of mothers and infants and/or transforming childbirth locally, nationally or internationally.

Monica McLemore, RN, MPH, Ph.D., Associate Professor, UCSF School of Nursing
Monica McLemore is an Assistant Professor, Family Health Care Nursing Department at University of California San Francisco and Research Scientist, Advancing New Standards in Reproductive Health. Her program of research is focused on understanding the factors that contribute to inequities in women’s reproductive health and justice. The goals of Dr. McLemore’s research are threefold: 1) to improve patient outcomes, 2) to improve access to care, and 3) to improve patients’ experiences of their care. Reproductive Justice (RJ) is an intersectional framework that serves as a roadmap that guides all of my research, which can be categorized into four content areas area, namely, interrogating the context and content of care, evaluating providers of care, determining baselines of quality care, and generating evidence to inform policies that impact care.
Lifetime Achievement Award: Geraldine Perry-Williams, PHN, MSN, former MCAH Director, City of Pasadena Public Health Department
Description: To honor a person who has shown many years of dedication, perseverance and service to mothers and infants & the birth professional community. This category can be given to someone posthumously or living.

Geraldine Perry-Williams, PHN, MSN, former MCAH Director, City of Pasadena
Geraldine Perry-Williams, PHN, MSN believes if women are healed from their hurts and provided the resources they need, then we will see change in our families, our communities and in our children. Geraldine is a public health nurse and is passionate about improving the health and well-being of underserved populations in urban communities to help them reach their highest potential, heal from their trauma and produce healthy babies and children, despite societal obstacles that are placed in their way. Her work over the last 30 plus years, in service to her community, has focused on conducting outreach and education to women, children and families, community engagement and developing and, conducting trainings that address trauma, toxic stress and environmental toxins, self-care and various other titles. Geraldine served the citizens of the greater Pasadena area working for the City of Pasadena Public Health Department for 24 years in several capacities such as the Maternal Child and Adolescent Health Director, Perinatal Services Director and Childhood Lead Program Director, Black Infant Health Coordinator. She initiated numerous Call to Actions to bring awareness to the community of issues facing the MCH population. She has provided input on a state and national level working on various executive committees and boards. She is a fellow from the University of North Carolina MCAH Public Health Leadership institute. She has devoted her life and career to healthy birth and social justice issues and speaking up for those who don’t feel they have a voice.
Most Audacious Award: Chemin Perez, LM, CPM, Founder, Nueva Vida Parteria/New Life Midwifery & Arcadia Birth Center
Description: To honor a MCH or Childbirth professional who has shown remarkable courage and boldness to change childbirth or maternity care.

Chemin Perez, LM, CPM, Arcadia Birth Center/Nueva Vida Parteria
Chemin Perez is a California Medical Board Licensed Midwife and Certified Professional Midwife accredited by North American Registry of Midwives. She is a 2014 graduate of the National College of Midwifery. She founded the Arcadia Birth Center in Arcadia, CA in 2016. She is a midwifery preceptor for the National College of Midwifery and mentors midwifery students and serves on the Midwifery Advisory Committee of the California Medical Board. Chemin chose to have a home birth attended by a midwife when she was pregnant with her first child at the age of 16. Her experience was life changing. Chemin was treated with such respect, love and care throughout her pregnancy by her midwife, it influenced her to pursue her journey as a midwife. She is a mother of eight children and is a grandmother of three. Chemin is the first Licensed Midwife of Mexican-American decent in Los Angeles and is bi-lingual in Spanish. Chemin comes from a long line of midwives and Curanderas in Mexico. She was inspired to become a midwife by her Abuela. Chemin worked as a Doula for several years prior to becoming a midwife.
Dr. Paul M. Fleiss MD, MPH; Future Leader Award: Haize Hawke, CD, Doula & Student Midwife and Renae Morales, Student Midwife & Doula
Description: To honor an up and coming professional/student in the field who shows great promise and aptitude to make a significant change in society or the field of medicine, midwifery, nursing or doula support. This award is given in honor of beloved Los Angeles pediatrician Paul M. Fleiss, MD, MPH, who inspired and supported many maternal-child health practitioners and leaders.

Haize Hawke, Student Midwife
Haize Hawke, Certified Doula and a Student Midwife, Life Coach, Mentor and Community Leader, is an advanced Doula who honors birth as a sacred Rite of Passage and the womb as it’s Temple. Haize supports the belief that pregnancy is a spiritual, emotional, mental and physical journey.For over seventeen years Haize has been and continues serve the Los Angeles community as a youth mentor. She guides young men and women through self-work to find their own purpose and passion for life. Standing on the structure of embracing the masculine and the feminine, she works with them on self-love – the key to everything. Haize is a student midwife with Childbirth at Home- A Labor of Love.

Renae Morales, Student Midwife
Renae Morales has 15 combined years of experience as an Bradley Method educator, DONA trained birth and postpartum doula, and postpartum service provider, Renea Morales’ knowledge and experience working within the birth world focuses on educating moms and families on many ways to birth, empowering them to have a voice and positive birth experiences as they bring their children into this world. She works tirelessly to make an impact to improve the outcomes of birth with special focus on the various communities; single moms, families of color, VBAC moms where many systems do not offer the support to them to achieve their goals.
These students have a commitment to working with disadvantaged persons, and have shown exemplary leadership skills.
Visionary Of The Year: J. Chinyere Oparah, Ph.D., Activist-Scholar, Social Justice Educator and Community Organizer & Founder, Black Women Birthing Justice and Provost and Dean of the Faculty, Mills College
Description: For exemplar and paradigm-shifting models of childbirth and/or maternal and infant health, causing significant social change or improvement in childbirth nationally, locally or internationally.

Chinyere Oparah, Ph.D., Founder, Black Women Birthing Justice & Provost and Dean of the Faculty, Mills College
Julia Chinyere Oparah is a collaborative leader, activist scholar, social justice educator and experienced community organizer, who is dedicated to producing critical scholarship in the service of progressive social movements. Oparah is an African diaspora specialist, whose interests span a number of different social concerns, including activism by women of color, violence against women, women and the prison-industrial complex, restorative justice, queer and transgender liberation, race and adoption, research justice and birth activism. Her most recent book, Birthing Justice: Black Women, Pregnancy and Childbirth, coedited with Alicia D. Bonaparte, places black women at the center of debates around childbirth and foregrounds their role in the emerging birth justice movement. She is currently working with the grassroots community organization Black Women Birthing Justice on a participatory action research project about black women’s experiences of pregnancy and childbirth.
RATIONALE FOR CONFERENCE
Worse birth outcomes exist in communities of color, and lower-income communities. During pregnancy, place and  ethnicity matters. It shapes how healthy a mother will be and how well or poorly her child will fare. Furthermore, reproductive rights and women’s rights in the U.S. have primarily focused on access to contraception and safe abortion, gender-based violence and trafficking. Though the fact that the other aspect of reproduction is pregnancy and childbirth, this aspect has not been the focus of reproductive and women’s rights activists.Woman-abuse not only takes the form of rape and domestic violence, but also obstetrical violence occurs more frequently than one might expect. This is an area where those who are concerned about violence against women must also focus. Additionally, LGBTQ activists have not as often focused on the rights of childbearing persons within their communities. This forum will shine a light on some of the issues faced by LGBTQ persons during childbirth.
ethnicity matters. It shapes how healthy a mother will be and how well or poorly her child will fare. Furthermore, reproductive rights and women’s rights in the U.S. have primarily focused on access to contraception and safe abortion, gender-based violence and trafficking. Though the fact that the other aspect of reproduction is pregnancy and childbirth, this aspect has not been the focus of reproductive and women’s rights activists.Woman-abuse not only takes the form of rape and domestic violence, but also obstetrical violence occurs more frequently than one might expect. This is an area where those who are concerned about violence against women must also focus. Additionally, LGBTQ activists have not as often focused on the rights of childbearing persons within their communities. This forum will shine a light on some of the issues faced by LGBTQ persons during childbirth.
Facts:
- Black women have the highest rates of cesarean section followed by Hispanic women in the USA.
- Between 1999 and 2004 in Los Angeles County, the Maternal Mortality rate of African-American women rose 157%, to 45.6 per 100,000 live births, more than double the rise among Caucasian women. Over the same period there was also an unexpected 765% surge in the maternal mortality rate of Asian/Pacific Islanders.(LABBN, 2009).
- There has been a rising cesarean section rate in the USA in the past decade in part due to repeat cesareans and low rates of Vaginal Birth After Cesarean (VBAC). Vaginal birth after cesarean (VBAC) were relatively few and decreased from 3.75% in 1999 to 1.41% in 2005 (p<0.0001). This represents a significant 62% decrease in VBAC over the study period (Maternal Quality Indicators Project, 2011, p. 38 ).
- In California in 2012-2014, Black women have the highest rates of cesarean section, as they do nationally. In California, the rate is 37.7% for Blacks compared to 32.4% for Whites, and 33.1% overall in the state. The US overall rate is 32.6%, and for Black women it is 35.5% and 32% for White women from 2012-2014. (National Center for Health Statistics, 2017).
- The cesarean section rate by Los Angeles Service Planning Area ( SPA ) is 37% in SPA 7 compared to 34.8 in Metro LA (SPA 4), which is the lowest in the county and 38.3% in the San Fernando Valley, which is 2nd highest. The highest in the county is 39% in San Gabriel Valley(California Department of Public Health, Center for Health Statistics, OHIR Vital Statistics Section, 2003-2012).
- Maternal Mortality is 4-5 times higher for African-American women than White women in the USA. This is the leading perinatal indicator between Blacks and Whites a disparity has not changed in 5 decades (APHA, 2010).
- In 2006, African-American women in California were more than three times as likely to die from pregnancy-related causes as Caucasian women.
- Certain Los Angeles zip codes have 3-4 times higher rate of Maternal Mortality than others.
- In Los Angeles County, in 2007, 11 Hispanic women and 7 African American women died during pregnancy, childbirth, or puerperium (LABBN, 2009).
- Hispanic women make up 46% of all women in LA County, but 50% of all maternal deaths.
- African-American women make up 9.2% of all women in LA County, but 31.8% of all maternal deaths.
- White women make up 28.9% of women in LA County, but only 4.5% of maternal deaths.(California Department of Health Services, Center for Health Statistics, Vital Statistics, 2007 from: LA Best Babies Network).
- In LA County, according to LA Best Babies Network’s 2009 report, the leading cause of maternal death is obstetric hemorrhage.
- American-born Black women are twice as likely than American-born White women to give birth too early too babies that are too small and who are twice as likely to die within the first year of life. This is not a result of lack of prenatal care, poverty, or unhealthy lifestyles. Even Black women who have healthy behaviors and are have a high level of education and wealth, are twice as likely to give birth too early at a rate double the rate of White woman with less than a high school diploma (Lu & Halfon, 2003).
This event explored the political, social, systemic and historical reasons for maternal-infant health inequities and disparities in communities of color, from the voices of women themselves. There are various factors that contribute to maternal mortality, prematurity and high cesarean rates for women of color.
“This is not just a health care crisis–it is a public health emergency” (Amnesty International, 2010).
Socioecological Model
At this event, we will use the Socioecological Model to explore the reasons and a opportunities for intervention to improve birth outcomes and quality of care. In this model, various domains of influence are described, both macro and micro, upon a disease condition or health problem. Understanding of these spheres of influence allow the practitioner or advocate to develop specific interventions geared at each or some of these domains.
These include:
Intrapersonal/individual factors: influence behavior in predisposing ways such as knowledge, attitudes, beliefs of the individual childbearing person..

The Socioecological Model as applied to violence against women and girls, however it applies to Obstetrical Violence as well. (Source: The Lancet, retrieved from: http://www.thelancet.com/cms/attachment/2020894921/2041097832/gr2.jpg)
Interpersonal factors: these are family members, peers, health professionals, teachers, counselors, etc. that either foster or hinder interpersonal growth or healthy behavior.
Institutional and organizational factors: these are hospitals, schools, churches, workplaces, etc. that create rules, regulations, policies, and informal structures that constrain or promote healthy behaviors or foster diseases or health disparities.
Community factors: these are formal or informal social norms and customs or cultural practices that exist among groups, families or organizations such as workplaces, schools, religious institutions, that can hinder or  help individuals perform healthy behaviors or perpetuate a disease or health problem.
Society Factors: These are public policies, laws, political climate or political ethos, that regulate or support health actions and practices for fostering or inhibiting changes in health behavior, health problem or disease.
Using a the Socioecological Model and a human rights framework, participants learned about each of the fundamental rights of childbearing persons, including the right of informed consent and refusal, privacy, equal treatment, and discussed opportunities for intervention at various levels and domains of influence. The panel discussion by reproductive justice and maternal health leaders discussed the historical and cultural factors which have kept ethnic perinatal health disparities intransigent for decades.
Participants will participated in exercises to explore with practical strategies and increase awareness of how to foster respectful and inclusive care and engender a more equitable maternity care system for all. When people have a sense of hope about their ability to change their world, they become encouraged and hopeful and this improves health and well-being by lowering the stress and anxiety that arises out of hopelessness and feelings of helplessness. A model of community empowerment that links all three levels–individual, organizational/institutional and community– provides the most effective means to collectively provide the support and control necessary to develop needed skills, resources, and change (Isreal, et. al. 1994). Furthermore, what is most effective in alleviating the effects of stressor exposure is when individuals perceive greater control over the stressor (Compass et al. 1991, as reported in Brenner, 2013).
References
1.Amnesty International USA (2010). Deadly Delivery: The Maternal Health Care Crisis in the USA. Retrieved from: http://www.amnestyusa.org/sites/default/files/pdfs/deadlydelivery.pdf
2. Brenner, A. B., Zimmerman, M. A., Bauermeister, J. A., & Caldwell, C. H. (2013).Neighborhood context and perceptions of stress over time: An ecological model of neighborhood stressors and intrapersonal and interpersonal resources.American Journal of Community Psychology, 51(3-4), 544-556.
3.Boumediene, S, Chow, J., Fridman,M, Gregory K, Korst, L., Lu, MC, et. al.(2011). Trends in Maternal Morbidity in California 1999-2005, Retrieved from: https://archive.cdph.ca.gov/programs/mcah/Documents/MO-CAPAMR-TrendsinMaternalMorbidityinCalifornia-1999-2005-TechnicalReport.pdf
4,California Department of Public Health, Center for Health Statistics, OHIR Vital Statistics Section. (2003-2012). Cesarean Section, Retrieved from: http://publichealth.lacounty.gov/mch/fhop/FHOP2012/C-section_2012_FINAL.pdf
5.California Department of Health (2016). 1991-2012 Birth Cohort and Birth Statistical Master Files State of California DPH. Retrieved From: http://www.ipodr.org/dashboard/dash.html
6.Los Angeles Department of Public Health (2017). SPA Areas by zip code. Retrieved from: http://publichealth.lacounty.gov/
7.Israel, B.A., Checkoway, B., Schulz, A., & Zimmerman, M. (1994). Health education and community empowerment: Conceptualizing and measuring perceptions of individual, organizational, and community control. Health Education and Behavior, 21(2), 149-170.
8.Lu MC, Halfon N (2003) Racial and Ethnic Disparities in Birth Outcomes:A Life Course Perspective. Maternal and Child Health Journal; 7(1):13-30.
9.Boumediene, S, Chow,J,Fridman,M, Gregory K, Korst, L., Lu, MC, et. al.(2011). Trends in Maternal Morbidity in California 1999-2005, Retrieved from: https://archive.cdph.ca.gov/programs/mcah/Documents/MO-CAPAMR-TrendsinMaternalMorbidityinCalifornia-1999-2005-TechnicalReport.pdf
10.California Department of Public Health, Center for Health Statistics, OHIR Vital Statistics Section. (2003-2012). Cesarean Section, Retrieved from: http://publichealth.lacounty.gov/mch/fhop/FHOP2012/C-section_2012_FINAL.pdf
11.California Department of Health (2016). 1991-2012 Birth Cohort and Birth Statistical Master Files State of Californi DPH. Retrieved From: http://www.ipodr.org/dashboard/dash.html
12.Los Angeles Department of Public Health (2017). SPA Areas by zip code. Retrieved from: http://publichealth.lacounty.gov
13. Journal of Perinatal Education, Supplement (Winter, 2007), Evidence Basis for Mother-Friendly Childbirth Initiative, Retrieved from http://www.motherfriendly.org/Resources/Documents/CIMS_Evidence_Basis.pdf
14, Kozhimannil, KB, Vogelsang, A, Hardeman, R, Prasad, S (2016).Disrupting the Pathways of Social Determinants of Health: Doula Support during Pregnancy and Childbirth, J Am Board Fam Med vol. 29 no. 3 308-317 doi: 10.3122/jabfm.2016.03.150300, Retrieved from: http://www.jabfm.org/content/29/3/308.full.pdf+html
15.National Center for Health Statistics, final natality data. Retrieved January 16, 2017, from www.marchofdimes.org/peristats.
16.Racial and Ethnic Disparities in Birth Outcomes (Fact Sheet), Retrieved from: www.marchofdimes.org/Racial-and-Ethnic-Disparities_feb-27-2015.pdf
17.Reese, P. Interactive: See C-section rates at every California hospital (2011). The Sacramento Bee, Office of Statewide Health Planning and Development. Retrieved from: http://www.sacbee.com/site-services/databases/article4129666.html



































